Against the back and forth debates regarding the efficacy of Covid-19 vaccines, experts met recently to rub minds on the subject matter as SADIQ ABUBAKAR reports.
The safety, efficacy and effectiveness of COVID-19 vaccines in the North-east and other northern parts of the country has remained a subject of discussion at several fora, various community groups and leaders with little/ unprofessional answers from medical and health experts.
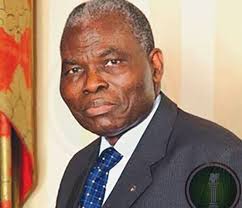
To that extent, recent investigations have proved that the COVID-19 vaccines being approved and recommended by the federal government and World Health Organisation (WHO) for Nigerians, (AstraZeneca and Moderna Covid-19 vaccines) are safe, effective and life-saving. This is according to the vice chancellor, Federal University of Kashere Gombe, Professor Umaru A Pate.
The debates
The resource person, Professor Pate who is also a professor of Human Communication and a veteran journalist stated this in his paper presentation titled: ‘Debunking Rumours and Misconceptions on Use and Safety of COVID-19 Vaccines’ during a recent two-day media dialogue on demand creation on COVID-19 vaccines in Kano.
On his part, Dr Murtala Gadanya of Aminu Kano General Hospital who is also a senior lecturer in the Department of Pharmacology and Therapeutic, Bayero University Kano in his paper presentation during the two- day media dialogue on ‘Demand Creation on COVID-19 Vaccines’ said that once the study is completed, the numbers of sick people in each group are compared in order to calculate the relative risk of getting sick depending on whether or not the subjects received the vaccine.
“COVID-19 Vaccine’s efficacy is measured in a controlled clinical trial and is based on how many people who got vaccinated developed the ‘outcome of interest’ (usually disease) compared with how many people who got the dummy vaccine developed the same outcome.
“From this, we get the efficacy which is a measure of how much the vaccine lowered the risk of getting sick. If a vaccine has high efficacy, a lot fewer people in the group who received the vaccine got sick than the people in the group who received the dummy vaccine.
“Like all vaccines, they do not fully protect everyone who is vaccinated and we do not yet know how well they can prevent people from transmitting the virus to others. So as well as getting vaccinated, we must also continue with other measures to fight the pandemic,” Gadanya said.
According to him, all COVID-19 vaccines approved by WHO for emergency use listing have been passed through randomised clinical trials to test their quality, safety and efficacy.
“Although, some are yet to be approved, vaccines are required to have a high efficacy rate of 50% or above. After approval, they continue to be monitored for ongoing safety and effectiveness.
“But one could be able to ask to know the difference between efficacy and effectiveness. For example, let’s imagine a vaccine with a proven efficacy of 80% which means that out of the people in the clinical trial, those who received the vaccine were at an 80% lower risk of developing disease than the group who received the placebo.
“This is calculated by comparing the number of cases of disease in the vaccinated group versus the placebo group. An efficacy of 80% does not mean that 20% of the vaccinated group would become ill,” Murtala said.
He said further that, “Vaccine effectiveness is a measure of how well vaccines work in the real world. Clinical trials include a wide range of people, a broad age range, both sexes, different ethnicities and those with known medical conditions.
“But they cannot be a perfect representation of the whole population. The efficacy seen in clinical trials applies to specific outcomes in a clinical trial. “Effectiveness is measured by observing how well the vaccines work to protect communities as a whole. Effectiveness in the real world can differ from the efficacy measured in a trial because we can’t predict exactly how effective vaccination would be for a much bigger and more variable population getting vaccinated in more real life conditions,” Dr Gadanya said.
He further noted that vaccine protection and timing offer strong protection, but that protection takes time to build. People must take all the required doses of a vaccine to build full immunity.
“For two-dose vaccines, it only give partial protection after the first dose and the second dose increases that protection. It takes time before protection reaches its maximum level a few weeks after the second dose.
“For a one-dose vaccine, people would have built maximum immunity against COVID-19 a few weeks after getting vaccinated.
“Vaccine protection and infection can stop most people from getting sick with COVID-19, but not everyone,” Gadanya added.
“Even after someone takes all of the recommended doses and waits a few weeks for immunity to build up, there is still a chance that they can get infected. Vaccines do not provide full (100%) protection; so ‘breakthrough infections’, where people get the virus, despite having been fully vaccinated would occur.
“If vaccinated people do get sick, they are likely to have milder symptoms. In general, It is very rare for someone vaccinated to experience severe illness or die”, Murtala said.
The professional pharmacologists also explained that COVID-19 vaccines are crucial tools in the pandemic response and protect against severe disease and death. He is of the views that vaccines provide at least some protection from infection and transmission, but not as much as the protection they provide against serious illness and death. More evidence is needed to determine exactly how well they stop infection and transmission.It is advised that after being vaccinated, individuals should continue taking simple precautions, such as physical distancing, wearing a mask, keeping rooms well ventilated, avoiding crowds, cleaning hands, and coughing into a bent elbow or tissue. It is advisable to get tested if one is sick even if one is vaccinated.
Vaccine protection and variants When cases increase and transmission accelerates, it’s more likely that new dangerous and more transmissible variants emerge, which can spread more easily or cause more severe illness.
He said, “Based on what we know so far, vaccines are proving effective against existing variants, especially at preventing severe disease, hospitalisation and death. However, some variants are having a slight impact on the ability of vaccines to guard against mild disease and infection.”Vaccines are likely staying effective against variants because of the broad immune response they cause, which means that virus changes or mutations are unlikely to make vaccines completely ineffective.
He said, “WHO continues to constantly review the evidence and would update its guidance as we find out more. For the latest updates on what we know about the COVID-19 variants, read our latest weekly epidemiological updates and our explainer on ‘the effects of virus variants on COVID-19 vaccines.”
It has been observed that one of the best ways of guarding against new variants is to continue applying tried-and-tested public health measures and rolling out vaccines. All COVID-19 vaccines approved for emergency use listing by WHO have been thoroughly tested and proven to provide a high degree of protection against serious illness and death.
As stronger virus variants emerge, it’s important to take vaccine when it’s one’s turn.